Jun. 10, 2020
Summary
- Looking back at Japan’s response to Covid-19 up to the present, we see that the government has taken measures while altering its policies depending on how the virus has spread. This policy change, while still fundamentally entailing countermeasure strategies, has involved a shift in focus from preventing the virus from entering the country, to preventing it from spreading, and finally to preventing a severe spread, with various measures having been taken thus far. Although in some ways Japan’s countermeasures have yielded favorable results compared to other countries so far, we must also accept as fact that some unexpected challenges have arisen that cannot be handled with our existing policy and regulatory frameworks.
- One major factor behind these challenges is the difficulty involved in determining asymptomatic infection and whose illnesses will worsen. There are two aspects to Japan’s success in controlling such a virus through countermeasures, namely our handling of supply-side problems such as medical facilities and medical workers, and our response to demand-side problems, e.g. the number of infected persons and those suspected to be infected.
- This paper focuses on the response made for handling infected and those suspected to be infected. The key points involved in demand-side issues here are as follows: appropriate government communications for enhancing citizens’ self-control following infection prevention and stratification; and immediate construction of a framework/system that can identify infections while valuing human rights. We also wish to suggest that the use and application of health and medical information could be an extremely effective solution to these challenges.
- Taiwan has garnered the world’s attention for its superlative handling of Covid-19, but its efforts were made possible by the use of health and medical information platforms that Taiwan has been developing for a long time.
- In Japan as well, the construction of health and medical information platforms is underway, yet for Japan to learn from Taiwan’s Covid-19 response and develop platforms with even greater value, there likely needs to be information sharing with various systems other than those for health/medical information, such as disaster information systems.
Japan’s Covid-19 Measures Have Been Implemented with a Flexibly Shifting Focus Depending on the Spread of the Virus
Looking back at Japan’s response to Covid-19 up to the present, we see that the government has taken measures while altering its policies depending on the spread of the virus. This policy change, while still fundamentally involving basic response measures for countering the spread of Covid-19*1, has involved shifts in emphasis from preventing the virus from entering the country, to preventing it from spreading, and finally to preventing a severe spread, as seen in Fig. 1.
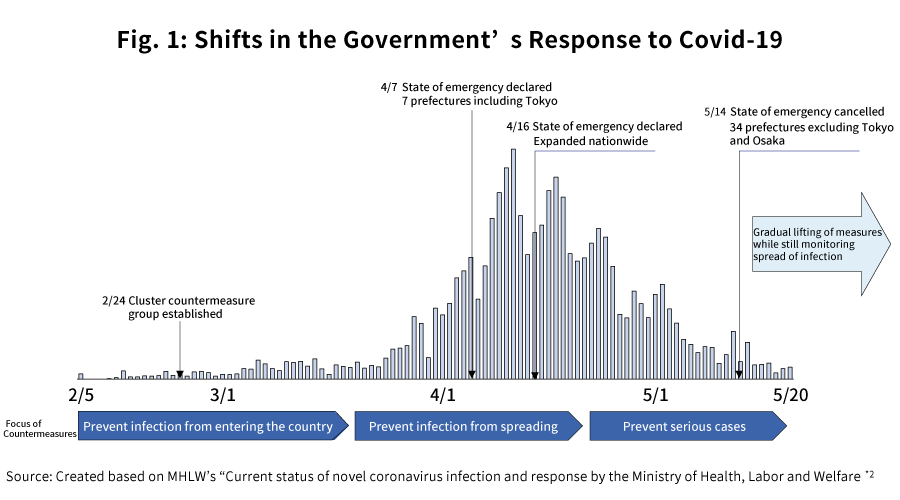
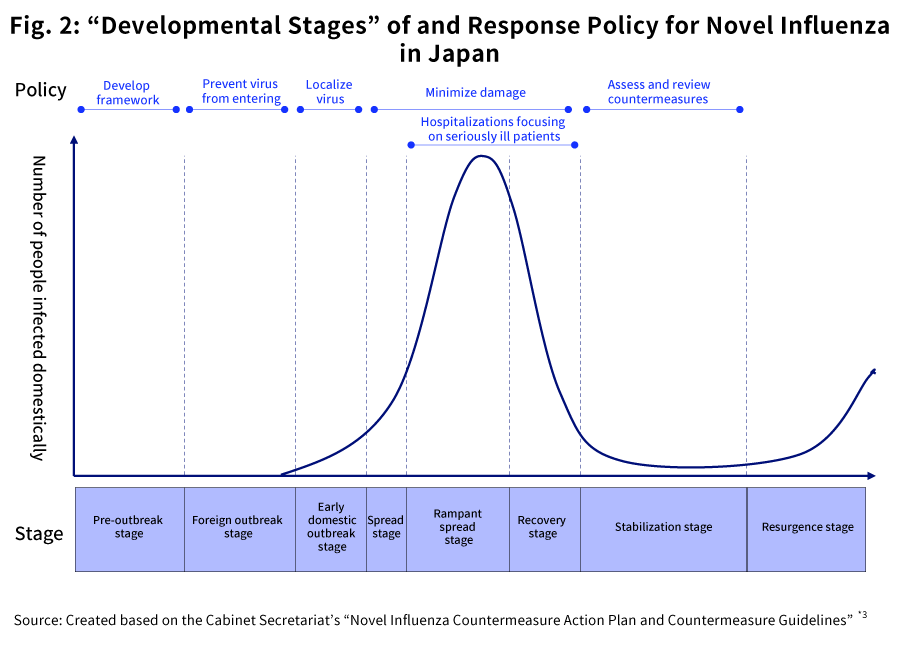
As shown in Fig. 2, when it comes to novel influenzas and other infectious diseases, Japan-specific expressions and countermeasure policies have been established by the government, separately from the pandemic influenza alert phases defined by the WHO. In the case of the current Covid-19 situation as well, based on this approach, countermeasures have been implemented under a policy of maximizing the effectiveness of infection prevention while also minimizing the impact on social an economic functions*1. From the foreign outbreak stage to the early domestic outbreak stage, emphasis was placed on preventing the disease from entering the country, with the purpose being to buy time for constructing an appropriate medical care system. Further, in the spread stage, the response was based on cluster countermeasures. The purpose of this was to prevent the spread of the illness via mass outbreaks and slow the speed of the rise in new patients, thereby lowering the peak and preventing the medical system from collapsing. And in the rampant spread stage, measures have been taken to ensure that appropriate resources were allocated to severely ill patients, through progression prevention and stratification.
While the Shifts in Japan’s Countermeasure Strategy Based on Covid-19’s Characteristics Have Yielded Some Excellent Results Compared to Foreign Countries, Other Unexpected Challenges Have Arisen that Cannot be Handled by Our Existing Policy and Regulatory Framework
According to a presentation by the Ministry of Foreign Affairs, the number of infected persons per 10,000 Japanese citizens was 1.34 as of the end of May, which was far lower than the numbers abroad in places such as the US (53.46) and England (41.06) at that time, and it can be read that efforts to hold down the number of infected persons up to the present at least have yielded some excellent results compared to foreign countries*4. Meanwhile, even amidst these results, we have to accept the fact that some unexpected challenges have also arisen which cannot be handled with our existing policy and regulatory framework. Moreover, updating our countermeasures so as to reflect these challenges going forward is arguably an important stance to take for the public and private sectors as well as the general population. Below, we provide a general outline of the issues needing to be discussed going forward that have arisen from the characteristics of Covid-19, as a basic list to frame the discussion.
Initial domestic outbreak stage- (1): Activity Restrictions Reliant on People’s Self Control
- Japan has not established any penal provisions or any other form of legal responsibility for citizens to quarantine themselves at home, and thus societal measures depend on people’s consciences to succeed. Japan’s Constitution at it currently stands does not contain any provisions about the state’s emergency powers, and so the government handles large-scale disasters and other events by enacting new laws on an individual basis. In this case, since there are no corresponding laws in place, it responded by partially amending the Act on Special Measures for Countermeasures against Novel Influenza, etc.
- Even at the stage where the infection was spreading, it was difficult to issue mandatory activity restrictions due to concerns over what legal foundation would underpin the legally binding force of such restrictions, and fears that these restrictions could become the basis for future exertions of state authority. For this reason, the extent to which the government could promote behavior modification through demands or requirements so as to control the virus’s spread became a vital issue.
- As a result of mask bulk buying etc., there was a nationwide shortage of materials for dealing with the spread of the virus. Although there were discussions about the government distributing cloth masks, the mask shortage persisted across the country. Finding ways to optimize the allocation of resources by the state, e.g. through the prevention of such bulk buying, became a challenge.
Initial domestic outbreak stage - (2): Reliably Identifying and Tracking Asymptomatic Cases
- Unlike previous infectious diseases (such as MERS or SARS), Covid-19’s characteristics make it easy to spread asymptomatically, and so some infected persons slipped through the cracks of our cluster countermeasures.
- Even after it became clear that Covid-19 lends itself to asymptomatic spread, since contact tracing etc. methods are fraught with personal privacy issues, it was difficult to put them into play quickly without an existing infrastructure, and it is possible that this aided the unmanaged spread of infection.
- Creating a public health system that can handle the disease’s propensity for high asymptomatic spread, in a way that is mindful of privacy and human rights, will be a challenge when it comes to similar infection control going forward.
Spread stage: Countermeasures for Preventing Spread in Hospitals
- The dramatic rise in cases of persons infected with Covid-19 temporarily caused chaos at medical institutions, and there were some such institutions where isolating infected persons (including those suspected to be infected) from normal patients did not work very well.
Rampant spread stage - (1): Optimal Allocation of Limited Medical Resources, e.g. PCR Tests
- There was a shortage of PCR test resources (e.g. kits, physicians/laboratory technicians), and thus medical institutions were forced to test only seriously ill patients or those who had clearly been in close contact with infected persons.
- The healthcare and pharmaceutical industries have traditionally operated according to careful protocols in the interest of safety, and thus it was difficult to secure medical supplies, medical workers, medical facilities and other medical resources and to make rapid improvements in the thick of the pandemic.
- Given these difficulties, the challenge became how to stratify patients, implement infection control, and distribute medical resources to seriously ill patients.
Rampant spread stage - (2): Management of Persons Receiving At-Home Care to Prevent In-Household Spreading
- Once stratification measures became possible, there were also many cases where it was difficult to isolate patients from cohabitants when administering at-home care, and although community acquired infections did drop, the percentage of in-household spreading increased.
- Although infected persons were encouraged to quarantine in hotels, these measures were not compulsory and patients could freely choose; thus, various circumstances including people’s family structures led more citizens to choose to receive at-home care, which may have aided the spread of the virus within households.
One major factor behind these challenges is the difficulty involved
in determining asymptomatic infection and whose illnesses will
worsen. That said, what exactly has Japan managed to achieve in
handling the virus by implementing controls? There are two aspects
involved here, namely, the handling of supply-side challenges such
as medical facilities and medical workers, and the handling of
demand-side challenges involving infected persons and those
suspected of being infected. Below, we discuss controlling the
demand involving infected persons and those suspected of being
infected.
The following are the key points regarding infection control for
Covid-19 patients and the general population, based on the issues
enumerated above.
“Appropriate government communications for enhancing citizens’ self-control following infection prevention and stratification”
- What to do to promote behaviors that prevent people from getting infected
- What to do to encourage those who are or who might be infected to receive the appropriate medical services while preventing further spread
- What to do to encourage medical care and stay-at-home behaviors that prevent further spread upon diagnosis/treatment while also not placing undue burdens on medical resources depending on the severity
“Immediate construction of a framework/system that can identify infections while valuing human rights”
- How can we visualize infection identification with consideration given to privacy?
- What kind of system do we need to immediately implement the above countermeasures as contingencies?
Regarding the points above, it is crucial that we advance these
efforts across all of Japan with constructive ideas taken from
various viewpoints. As one example of this, we believe the
leveraging of health and medical information currently underway in
Japan will prove useful. Not only is the use of health and medical
information platforms promising as a highly reliable basis for
communication between everyday people and medical workers, but by
creating a situation in which these platforms widely permeate
society as existing infrastructure, we could likely make them a
foundation for immediately responding even to unforeseen and sudden
pandemics.
In this paper, we summarize the fundamental elements of health and
medical information platforms for the advantageous use of health and
medical information. We then discuss the case of Taiwan, which has
gained notice for its superb handling of Covid-19, and report the
results of our investigation into the details of these platforms in
Taiwan, their usage during normal times, and what role they played
in combatting Covid-19. Finally, we consider the development status
of Japan’s health and medical information platforms, as well as how
we could become more effective in light of Taiwan’s example.
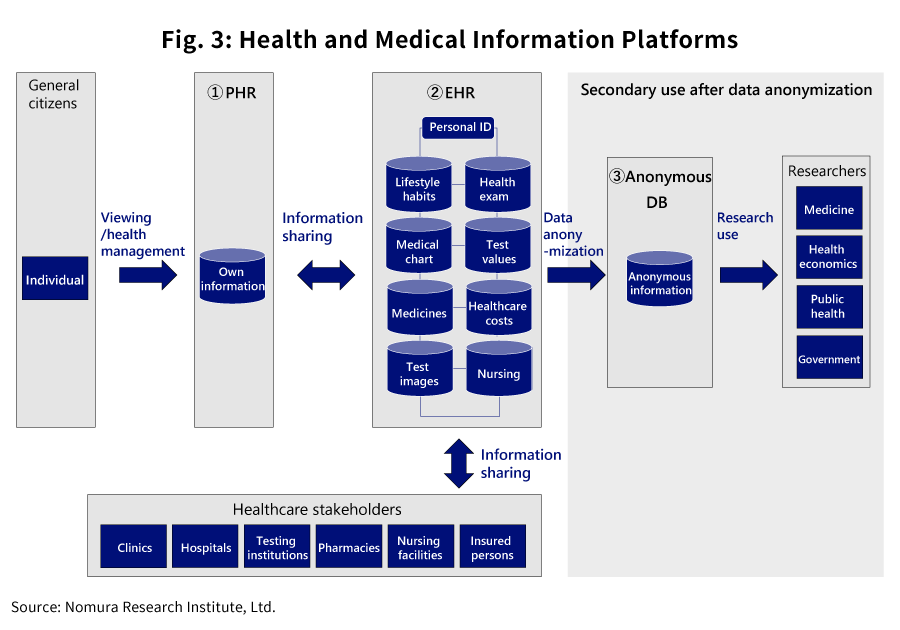
Health and Medical Information Platforms Consist of Three Elements: EHR (Electronic Health Records) for information sharing among healthcare stakeholders; PHR (Personal Health Records) for information sharing among patients and stakeholders; and anonymous databases (Anonymous DB) for public health and medical research purposes. When combined, these elements contribute to improving the quality of healthcare.
- At present, information pertaining to health and healthcare is managed using digitalized, structured databases all over the world, and efforts are being made to use these effectively.
- Efforts to effectively use health and medical information around the world consist of three elements as shown in Fig. 1, namely EHR (Electronic Health Records), PHR (Personal Health Records), and Anonymous DB. In this paper, these elements are collectively referred to as health and medical information platforms.
-
(1)
PHR (Personal Health Records)
- PHR is a system for managing the health and medical information of individuals, facilitating electronic information sharing between patients and healthcare stakeholders.
- In some cases, the information handled in PHR includes various kinds of information generated by healthcare stakeholders, as is true of EHR; it can also be other various information, with records that only cover lifestyle habits and vital information measured and inputted by patients themselves, which is then shared with medical workers.
- PHR plays two main roles. The first is to have patients understand their own health and medical information, and thereby gain a better grasp of their health conditions, which is helpful in promoting behavior modifications for maintaining and improving their health. The second is to share PHR information with healthcare stakeholders, helping the latter to better understand patients’ health conditions, and enabling patients to enjoy a higher quality of care.
-
(2)
EHR (Electronic Health Records)
- EHR is a system for linking health and medical information among various healthcare stakeholders, including among medical institutions, between such institutions and pharmacies, and among nursing facilities, thereby enabling information to be shared electronically beyond any organizational barriers.
- The information handled in EHR varies from country to country, but includes information about lifestyle habits, medical chart information, medical exams, prescribed medications, healthcare costs, test values, test images, and nursing-related information etc.
- This information is managed in an integrated way, linking shared personal IDs from the clinic, hospital, test facility, pharmacy, or nursing facility etc. from which it originated.
- EHR information can be shared among healthcare stakeholders regardless of any facility-related barriers, with various stakeholders involved in the care of a single patients quickly able to grasp in detail the condition of said patient, and thus it contributes to providing high-quality care including preventive care.
- Although EHR and PHR are discussed separately as concepts, in actuality there are platforms in place in various countries that possess both functions in combination.
- For instance, in countries where EHR development has historically been pursued first, it is common for EHR to be used as a foundation that enables it to be viewed not only by healthcare stakeholders, but also by patients via an app etc.
- Meanwhile, in countries where the focus has been on developing PHR systems, PHR serves as the foundation, with patients playing a main role in sharing their PHR information with the healthcare stakeholders assigned to them, meaning that PHR also serves a similar function to that of EHR.
-
(3)
Anonymous DB (Anonymous Databases)
- Anonymous DB are databases with which EHR or PHR information can be used not only for treating the patients themselves, but also for public health and medical research purposes.
- Because a patient’s information is used by persons other than the actual patient for research or other purposes not directly to the patient’s benefit, this information is often managed via anonymous databases, in the interest of personal information protection.
- The role of Anonymous DB is not simply to enable the primary use of information collected via EHR or PHR for patients themselves, but to actively facilitate secondary use of it for research and other purposes, ultimately leading to further quality enhancements for healthcare overall.
Taiwan has garnered the world’s attention for its superlative handling of Covid-19, but its efforts were made possible by the use of health and medical information platforms that Taiwan has been developing for a long time.
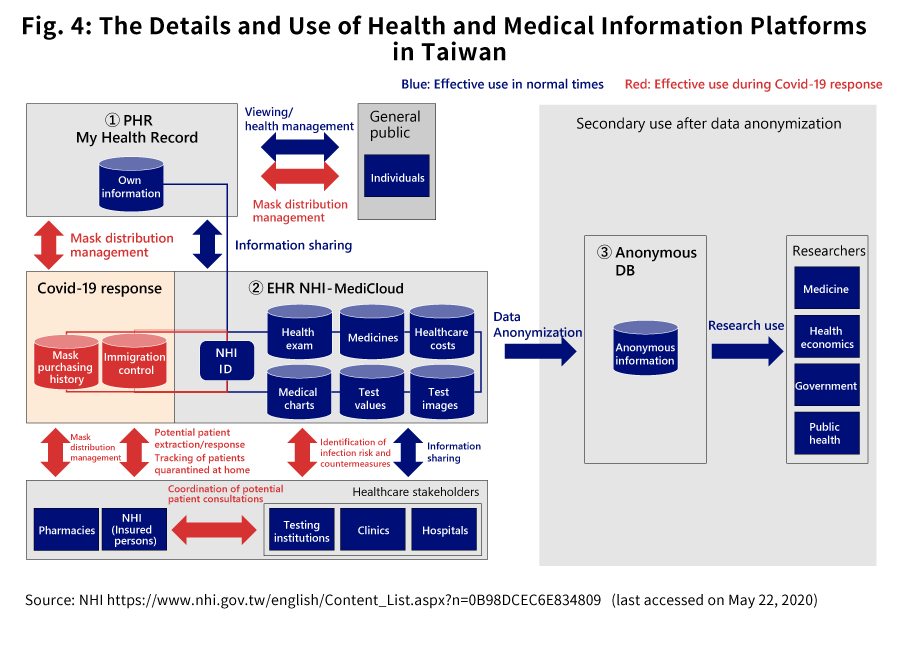
Taiwan is regarded as an advanced nation when it comes to developing health and medical information platforms. Regarding its handling of Covid-19, despite the country’s close proximity to China where the disease originated, it has had better results than Japan has, with the number of infected persons per 10,000 citizens was 0.19 as of the end of May*5, and its superlative efforts have frequently been cited in the news media. Below we discuss the nature of Taiwan’s health and medical information platforms and how they are used both during normal times and during the Covid-19 response.
-
(1)
Summary of Health and Medical Information Platforms Operated by Taiwan *6
-
PHR: My Health Bank
Taiwan’s PHR is known as My Health Bank, and like EHR, it is provided to the Taiwanese people by NHI. My Health Bank takes the form of a web service, allowing people to access (via their PCs or smartphones) records pertaining, for example, to their own hospitalization histories, dental care histories, allergies, healthcare expenses, surgical procedures, prescription medications, and the past three years’ worth of clinical test results. This system also includes a software development kit, and users can also request trustworthy third-party app developers to access their health and medical records to develop high-value-added services for them, so the system has high potential for expandability. -
EHR: NHI-MediCloud
Health insurance in Taiwan is a single-payer mandatory public insurance program, and 99% of the population is covered by its administrator NHI (National Health Insurance).
In Taiwan, NHI has played a leading role in constructing a cloud-based EHR system called NHI-MediCloud. Healthcare stakeholders can quickly obtain health information records for patients in their care from other hospitals or facilities through NHI-MediCloud, and this makes it possible to prevent duplicate medication or testing. The system permits medical imaging, health exam results, and even clinical test results to be shared, thereby ensuring the safety of treatments and medication administration, while at the same time reducing the waste of costly medical resources. -
Secondary Use of Anonymous DB
Since 2019, NHI has been operating a healthcare database in which all of the information is fully anonymous, including CT and MRI scans, clinical records, exams, and test charts. This database is used with permission from professional associations by public service bodies and academic R&D institutions (including profit-making businesses) for the purpose of developing AI functions and personalized healthcare, while still placing top priority on the protection of patient privacy. It is expected that this secondary use of anonymous DB will contribute to Taiwan’s biotechnology and healthcare industries and also lead to greater improvements in the quality of healthcare.
It should be noted that in Taiwan, the NHI IC card—a type of health insurance card—has been distributed to every person enrolled in public health insurance, i.e. to 99% of the population. This IC card has a person’s NHI ID (health insurance number) written on it, and functions as a personal identifier linked with health and medical information through NHI-MediCloud or My Health Bank. NHI ID also serves as personal identification when one browses My Health Bank.
-
PHR: My Health Bank
-
(2)
How It is Used in Normal Times
-
Healthcare quality improvements
As described earlier, these platforms can improve the quality of healthcare by facilitating information exchanges between healthcare stakeholders or between patients and healthcare stakeholders in NHI-MediCloud or My Health Record. -
Proven results in cutting medical costs
As is true in Japan, Taiwan is having to confront soaring medical costs and a shortage in fiscal resources as a result of its aging population, and the curbing of national medical expenditures has been one of the Taiwanese government’s main motives in undertaking the construction of NHI-MediCloud and My Health Record. In fact, it has been reported that from 2014 to 2017, the adoption of NHI-MediCloud successfully led to a roughly $9.63 million reduction in pharmaceutical costs through the detection and prevention of duplicate prescriptions, and to about $38.5 million less in testing costs by preventing redundant testing involving some 20 types of tests such as CTs and MRIs*7. -
Individual disease risk assessments and advice-based
promotion of national health
Research is being conducted for developing an algorithm that will assess a person’s risk of heart failure based on that person’s My Health Record information. Research is being done on ways of evaluating whether someone’s risk of heart failure is high or low in relation to the national average heart failure risk, with an alert then being sent to that individual through My Health Record. At the same time, efforts are underway to develop ways to give persons advice about what types of life changes can help improve their health (e.g. quitting smoking, exercising more), and even to provide necessary information for behavioral modifications to promote health, based on information regarding their lifestyle habits*8.
-
Healthcare quality improvements
-
(3)
How Taiwan’s Health and Medical Information Platforms Are Being Used to Combat Covid-19*9
-
Identifying and Tracking Patients Using Immigration Control
System and NHI-MediCloud Together
Because NHI-MediCloud and the country’s immigration control system have been linked together, doctors can verify the health conditions and travel histories of the patients in their care in a cohesive manner using NHI-MediCloud, while healthcare stakeholders on the frontlines can determine the risk of infection for the patients in their care and support relevant infection countermeasures and measures to prevent patients’ illnesses from getting more severe. Consequently, medical personnel can actively identify and track persons suspected to be infected or actual patients, without relying solely on patients’ declarations. -
NHI-MediCloud Intervention in Patients’ Medical
Consultations
In Taiwan, citizens listed on NHI-MediCloud as possibly being infected are screened and then introduced to local community research health centers designated by the government. This means that citizens do not have to search for health centers or medical institutions on their own, but rather can take action based on information distributed on medical information platforms. This system has thus prevented influxes of patients who are still only suspected of being infected from flooding advanced medical institutions and thereby impeding care for patients whose conditions are much more urgent. -
Effective Use of NHI IC Card and My Health Bank in Mask
Distribution
In Taiwan, when citizens log in to My Health bank using their NHI IC Cards, they can reserve and order masks at their pharmacies. In addition, the system limits the number of masks that can be purchased with a single NHI IC Card, as well as the available purchase dates, thus successfully preventing mask shortages caused by bulk-buying etc. By requiring NHI IC Cards to be displayed at the time of purchase, the system has made it possible nationwide to manage purchasing histories, purchasing eligibility, available purchasing dates, and distributed mask quantities on a per-person basis.
-
Identifying and Tracking Patients Using Immigration Control
System and NHI-MediCloud Together
In Japan as well, the construction of health and medical information platforms is underway, yet for Japan to learn from Taiwan’s Covid-19 response and develop platforms with even greater value, there likely needs to be information sharing with various systems other than those for health/medical information, such as disaster information systems.
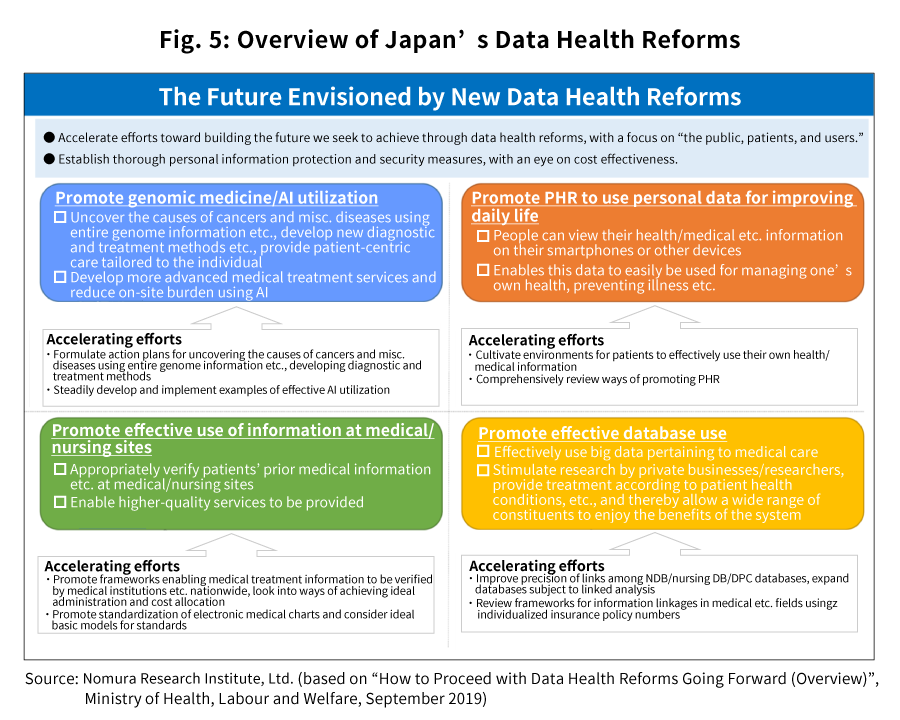
Japan can also be expected to develop and utilize health and medical
information platforms in the future. Under Japan’s data health
reforms, as shown in Fig. 5, efforts are underway to promote the use
of information corresponding to EHR at medical/nursing sites as well
as the use of PHR, and progress is also being made to advance the
use of databases and of AI for research purposes, for example. In
addition, there is talk of things like standardizing health and
medical information, and of linking information via insurance policy
numbers given to individuals as personal healthcare IDs. If these
efforts bear fruit in the future, Japan could very well join the
ranks of the leading countries when it comes to health and medical
information platforms.
The most fundamental elements in accelerating these efforts even
further are the following three points.
-
(1)
Faster dissemination of electronic medical charts
Naturally, in order for health and medical information to be circulated and effectively utilized via platform as it is in Taiwan, that information needs to in electronic form. In countries where PHR or EHR systems are in place, the rate of use of electronic medical charts at medical institutions—which are the primary source of medical information—is nearly 100%, and this enables medical information to be circulated as electronic data from the moment it is generated. Meanwhile, in Japan, the rate of use of electronic medical charts in general medical clinics or hospitals as of 2017 was not even 50%, and currently the majority of medical information remains in paper form *10. -
(2)
Vendor certification system based on standardization and structured format
Medical information becomes very difficult to utilize effectively if it cannot be used on a platform as a database. For this reason, it is normally preferable for medical information to be kept and circulated in a standardized, structure way. Meanwhile, electronic medical chart vendors not only in Japan but in other countries as well have developed electronic medical charts using proprietary company specifications, and this has made it difficult to circulate medical information among different vendors. However, in recent years, in countries that have developed PHR or EHR systems, the government or private groups have been making efforts to certify vendors by screening vendor systems in accordance with certain standards. These countries are combining their certified vendor systems with the incentive systems etc.described below, to produce incentives ensuring that vendors adhere to these standards. In Japan as well, amid data health reforms, standardization efforts continue to be discussed, and progress made in this area will surely be one of the keys to effectively utilizing health and medical information. -
(3)
Economic incentives for medical institutions to adopt and maintain EHR in accordance with standards
In order to promote the standardization of medical information, medical institutions must deploy vendor systems that conform to standard specifications. In countries that develop EHR systems with a sense of urgency, there are systems in place whereby medical institutions that employ certified vendors as described above can have their adoption expenses subsidized.
In addition to the above, in order to further enhance the value of
Japan’s health and medical information platforms, it would be
desirable to consider the potential for linking with other public
systems besides healthcare-related ones. One of the things that
Taiwan did particularly well in handling Covid-19 was to link the
health and medical information platforms it had been building to its
immigration control system and mask distribution system etc.,
allowing it to intervene in citizens’ activities in various respects
using IT systems and data. For Japan to develop more valuable health
and medical information platforms in the future, we believe it is
crucial to plan ways of linking information with other fields, such
as with disaster information sharing systems.
For example, Japan has disaster information sharing systems (e.g. L
Alert) that have been developed based on our experience with
frequent natural disasters including earthquakes and typhoons, and
these systems have even been highly regarded overseas for their
excellent disaster response. By linking information between these
systems and our health and medical information platforms, when an
earthquake strikes, we will be able to map out the regional seismic
intensity and damage situation along with population locations and
health/medical information, and this will enable the government to
ascertain the state and scope of the damage rapidly and in detail,
as well as effectively administer resources for relief.
-
*1.
Ministry of Health, Labour and Welfare, “Basic Management Policy for Covid-19 Infection Control Measures”
https://www.kantei.go.jp/jp/singi/novel_coronavirus/th_siryou/kihon_h_0504.pdf (last accessed: May 22, 2020) -
*2.
Ministry of Health, Labour and Welfare, “Current Status of Covid-19 Infection and the Ministry of Health, Labour and Welfare’s Response”
https://www.mhlw.go.jp/stf/houdou/index.html(last accessed: May 22, 2020) -
*3.
Cabinet Secretariat, “Novel Influenza Countermeasure Action Plan and Countermeasure Guidelines”
https://www.cas.go.jp/jp/seisaku/ful/keikaku/pdf/h29_koudou.pdf(last accessed: May 22, 2020) -
*4.
Ministry of Foreign Affairs,https://www.anzen.mofa.go.jp/covid19/pdf/graph_suii4.JPG(last accessed: May 31)
-
*5.
Taiwan Center of Desease Control
https://www.anzen.mofa.go.jp/covid19/country_count.html(last accessed: May 31) -
*6.
Executive Yuan,https://english.ey.gov.tw/News3/9E5540D592A5FECD/92cfaa8c-e224-4110-8d6e-dde134a7fa79 (last accessed: May 22, 2020)
-
*7.
Introduction to and Application Analysis of Taiwan’s NHI-MediCloud System, Journal of Service Science Research volume 11, pages93–115 (2019)
-
*8.
The development and implementation of stroke risk prediction model in National Health Insurance Service’s personal health record, J.-w. Lee et al. / Computer Methods and Programs in Biomedicine 153 (2018) 253–257
-
*9.
NHI
https://www.nhi.gov.tw/english/Content_List.aspx?n=0B98DCEC6E834809 (last accessed: May 22, 2020) -
*10.
Ministry of Health, Labour and Welfare https://www.mhlw.go.jp/content/10800000/000482158.pdf (last accessed: May 22, 2020)
Authors
Takuya Matsumoto
Global Manufacturing Industry Consulting Department
Nomura Research Institute
Takatoshi Hosoda
Global Manufacturing Industry Consulting Department
Nomura Research Institute
Atsushi Takada
Global Manufacturing Industry Consulting Department
Nomura Research Institute
Contact Us
Media Inquiries:
-
Corporate Communication Department
Nomura Research Institute, Ltd.
TEL: +81-3-5877-7100
Inquiries about the proposals:
-
Center for Strategic Management & Innovation
Nomura Research Institute, Ltd.